
DIABETES is a disease that occurs when your blood glucose, also called blood sugar, is too high. Blood glucose is your main source of energy and comes from the food you eat. Insulin, a hormone made by the pancreas, helps glucose from food get into your cells to be used for energy.

What is diabetes?
Diabetes mellitus, commonly referred to simply as diabetes, is a metabolic disease that causes high blood sugar.
The hormone insulin moves sugar from the blood into your cells to be stored or used for energy. With diabetes, your body either doesn’t make enough insulin or can’t effectively use the insulin it does make.
Untreated high blood sugar from diabetes can damage your nerves, eyes, kidneys, and other organs. But educating yourself about diabetes and taking steps to prevent or manage it can help you protect your health.
Types of diabetes
There are a few different types of diabetes:
Type 1: Type 1 diabetes is an autoimmune disease. The immune system attacks and destroys cells in the pancreas, where insulin is made. It’s unclear what causes this attack.
Type 2: Type 2 diabetes occurs when your body becomes resistant to insulin, and sugar builds up in your blood. It’s the most common type—about 90% to 95%Trusted Source of people living with diabetes have type 2.
Gestational: Gestational diabetes is high blood sugar during pregnancy. Insulin-blocking hormones produced by the placenta cause this type of diabetes.
A rare condition called diabetes insipidus is not related to diabetes mellitus, although it has a similar name. It’s a different condition in which your kidneys remove too much fluid from your body.
Each type of diabetes has unique symptoms, causes, and treatments.
Learn more about how these types differ from one another.
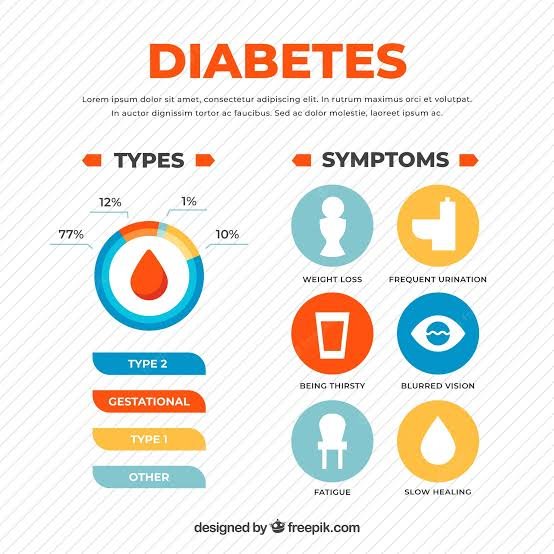
Symptoms of diabetes
Diabetes symptoms are caused by rising blood sugar.
General symptoms
The general symptoms of diabetes include:
increased hunger
increased thirst
weight loss
frequent urination
blurry vision
extreme fatigue
sores that don’t heal
Symptoms in men
In addition to the general symptoms of diabetes, men with diabetes may have:
a decreased sex drive
erectile dysfunction (ED)
poor muscle strength
Symptoms in women
Women with diabetes can have symptoms such as:
vaginal dryness
urinary tract infections
yeast infections
dry, itchy skin
Gestational diabetes
Most people who develop gestational diabetes don’t have any symptoms. Healthcare professionals often detect the condition during a routine blood sugar test or oral glucose tolerance test, which is usually performed between the 24th and 28th weeks of pregnancy.
In rare cases, a person with gestational diabetes will also experience increased thirst or urination.
The bottom line
Diabetes symptoms can be so mild that they’re hard to spot at first. Learn which signs should prompt a trip to the doctor.
Causes of diabetes
Different causes are associated with each type of diabetes.
Doctors don’t know exactly what causes type 1 diabetes. For some reason, the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas.
Genes may play a role in some people. It’s also possible that a virus sets off an immune system attack.
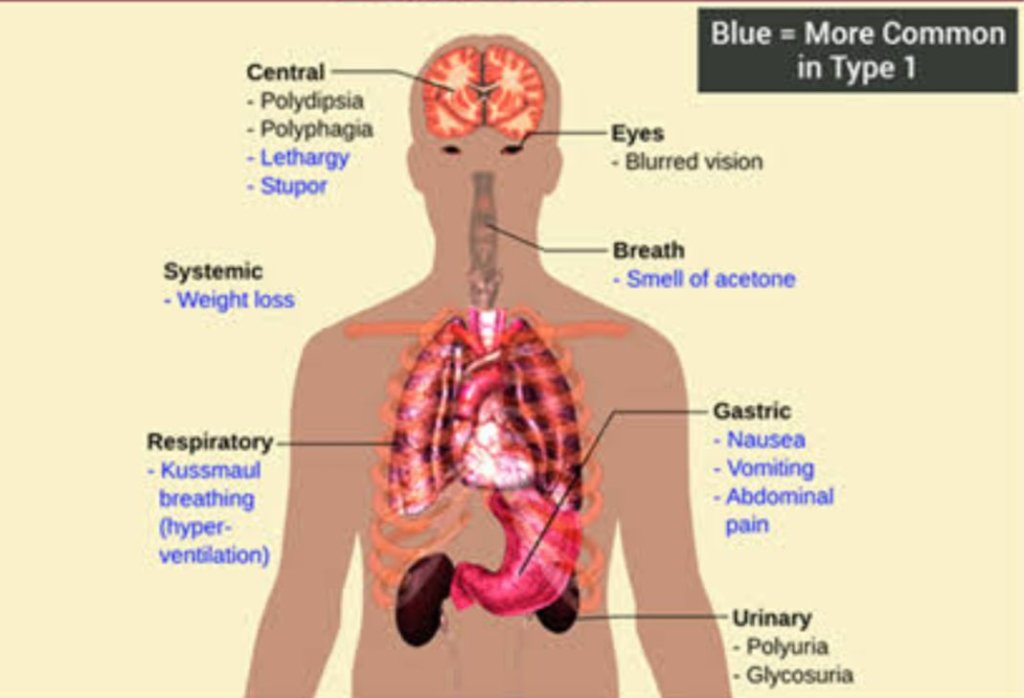
Symptoms of type 1 diabetes can include:
•extreme hunger
•increased thirst
•unintentional weight loss
•frequent urination
•blurry vision
•tiredness
•It may also result in mood changes.
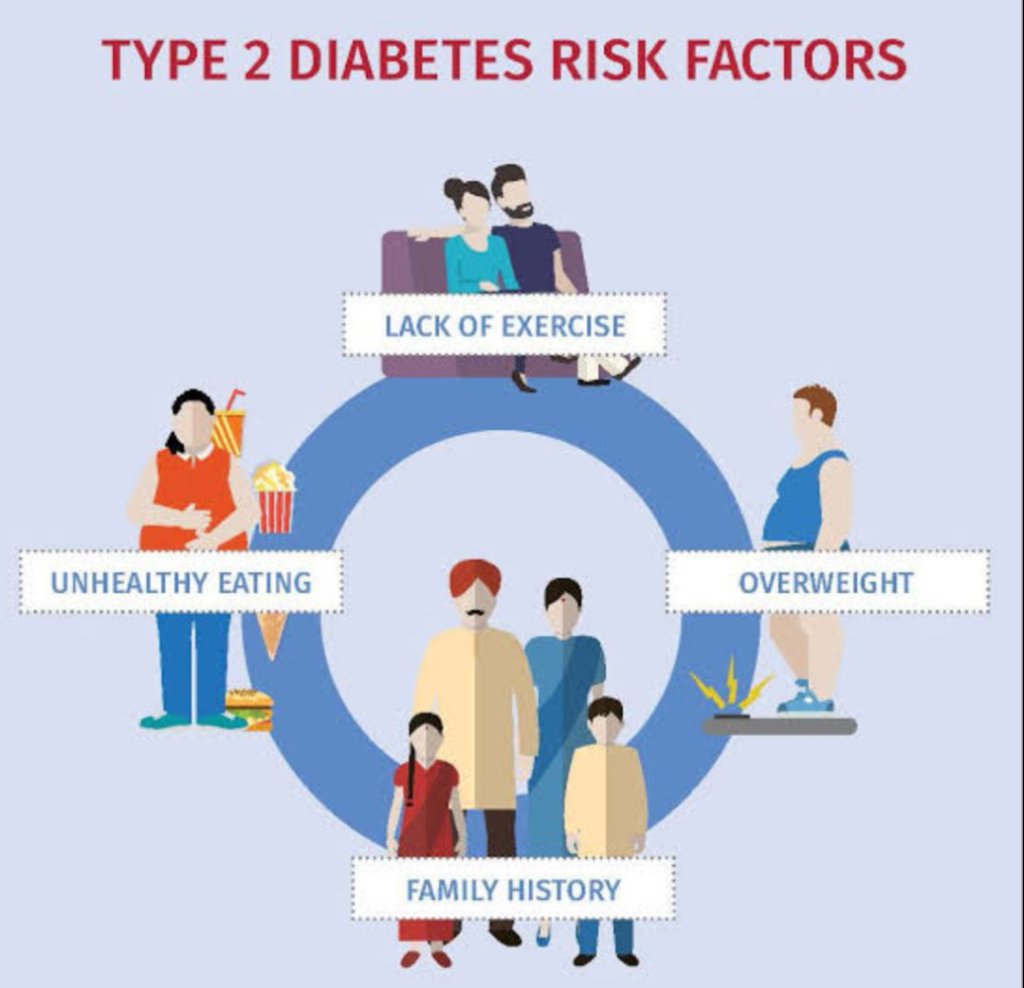
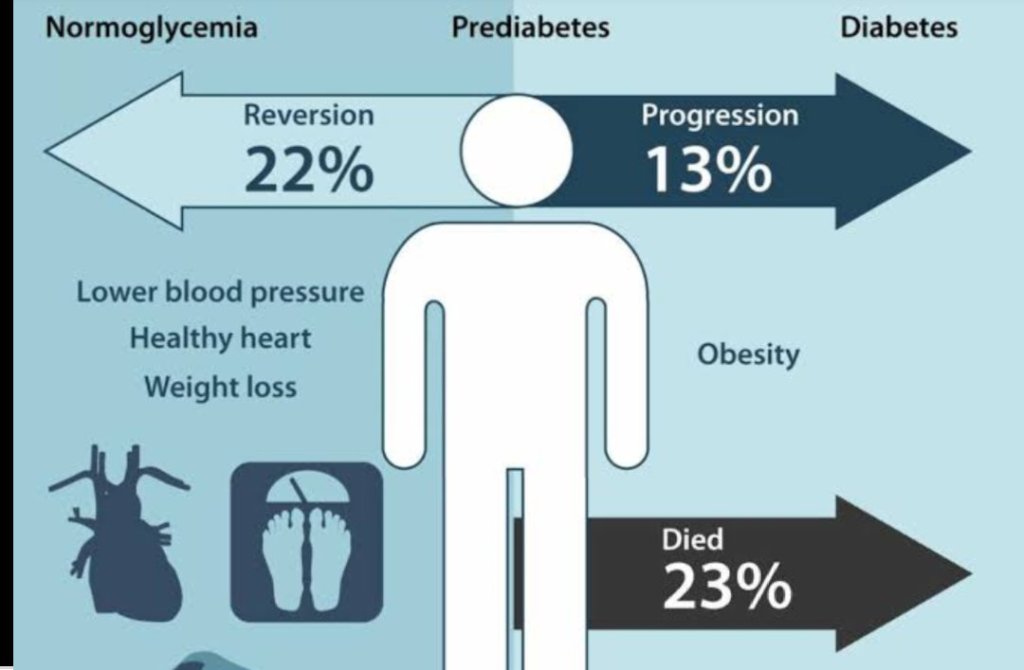
Type 2 diabetes stems from a combination of genetics and lifestyle factors. Having overweight or obesity increases your risk, too. Carrying extra weight, especially in your belly, makes your cells more resistant to the effects of insulin on your blood sugar.
This condition runs in families. Family members share genes that make them more likely to get type 2 diabetes and to be overweight.
Symptoms of type 2 diabetes can include:
•increased hunger
•increased thirst
•increased urination
•blurry vision
•tiredness
•sores that are slow to heal
It may also cause recurring infections. This is because high glucose levels make it harder for the body to heal.
PREDIABETES
Prediabetes is the term that’s used when your blood sugar is higher than expected, but it’s not high enough for a diagnosis of type 2 diabetes. It occurs when the cells in your body don’t respond to insulin the way they should. This can lead to type 2 diabetes down the road.
Gestational diabetes
Gestational diabetes occurs as the result of hormonal changes during pregnancy. The placenta produces hormones that make a pregnant person’s cells less sensitive to the effects of insulin. This can cause high blood sugar during pregnancy.
People who are overweight when they get pregnant or who gain too much weight during pregnancy are more likely to get gestational diabetes.
The bottom line
Both genes and environmental factors play a role in triggering diabetes.
Diabetes risk factors
Certain factors increase your risk for diabetes.
Type 1 diabetes
•You’re more likely to get type 1 diabetes if you’re a child or teenager, you have a parent or sibling with the condition, or you carry certain genes that are linked to the disease.
Type 2 diabetes
Your risk for type 2 diabetes increases if you:
•are overweight
•are age 45 or older
•have a parent or sibling with the condition
•aren’t physically active
have had gestational diabetes
•have prediabetes
have high blood pressure, high cholesterol, or high triglycerides
Type 2 diabetes also disproportionately affects certain racial and ethnic populations.
Adults who have African American, Hispanic or Latino American, or Asian American ancestry are more likely to be diagnosed with type 2 diabetes than white adults, according to 2016 research. They’re also more likely to experience decreased quality of care and increased barriers to self-management.
Gestational diabetes
Your risk for gestational diabetes increases if you:
•are overweight
•are over age 25
•had gestational diabetes during a past pregnancy
•have given birth to a baby weighing more than 9 pounds
•have a family history of type 2 diabetes
•have polycystic ovary syndrome (PCOS) The bottom line
Your family history, environment, and preexisting medical conditions can all affect your odds of developing diabetes.
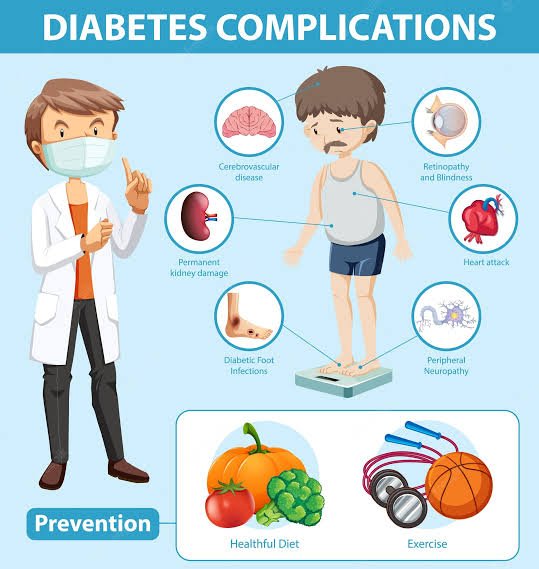
Diabetes complications
High blood sugar damages organs and tissues throughout your body. The higher your blood sugar is and the longer you live with it, the greater your risk for complications.
Complications associated with diabetes include:
•heart disease, heart attack, and stroke
•neuropathy
•nephropathy
•retinopathy and vision loss
•hearing loss
•foot damage, such as infections and sores that don’t heal
•skin conditions, such as bacterial and fungal infections
•depression
•dementia
Gestational diabetes
Unmanaged gestational diabetes can lead to problems that affect both the mother and baby. Complications affecting the baby can include:
•premature birth
•higher-than-typical weight at birth
•increased risk for type 2 diabetes later in life
•low blood sugar
•jaundice
•stillbirth
A pregnant person with gestational diabetes can develop complications such as high blood pressure (preeclampsia) or type 2 diabetes. You may also require cesarean delivery, commonly referred to as a C-section.
The risk of gestational diabetes in future pregnancies also increases.
The bottom line
Diabetes can lead to serious medical complications, but you can manage the condition with medications and lifestyle changes.
Avoid the most common diabetes complications with these helpful tips.

Healthy eating is a central part of managing diabetes. In some cases, changing your diet may be enough to manage the disease.
Type 1 diabetes
Your blood sugar level rises or falls based on the types of foods you eat. Starchy or sugary foods make blood sugar levels rise rapidly. Protein and fat cause more gradual increases.
Your medical team may recommend that you limit the amount of carbohydrates you eat each day. You’ll also need to balance your carb intake with your insulin doses.
Check out this guide to starting a type 1 diabetes diet.
Type 2 diabetes
Eating the right types of foods can both manage your blood sugar and help you lose any excess weight.
Carb counting is an important part of eating for type 2 diabetes. A dietitian can help you figure out how many grams of carbohydrates to eat at each meal.
In order to keep your blood sugar levels steady, try to eat small meals throughout the day. Emphasize healthy foods such as:
fruits
vegetables
whole grains
lean protein such as poultry and fish
healthy fats such as olive oil and nuts
Certain other foods can hurt efforts to manage your blood sugar.
Discover the foods you should avoid if you have diabetes.
Gestational diabetes
Eating a well-balanced diet is important for both you and your baby during these 9 months. Making the right food choices can also help you avoid diabetes medications.
Watch your portion sizes, and limit sugary or salty foods. Although you need some sugar to feed your growing baby, you should avoid eating too much. Check out other do’s and don’ts for healthy eating with gestational diabetes.
The bottom line
Work with a registered dietitian, if you have access to one. They can help you design an individualized diabetes meal plan. Getting the right balance of protein, fat, and carbs can help you manage your blood sugar.
Diabetes and exercise
Along with diet and treatment, exercise plays an essential role in diabetes management. This is true for all types of diabetes.
Staying active helps your cells react to insulin more effectively and lower your blood sugar levels. Exercising regularly can also help you:
reach and maintain a healthy weight
reduce your risk of diabetes-related health complications
boost mood
get better sleep
improve memory
If you have type 1 or type 2 diabetes, general guidance is to aim for at least 150 minutes of moderate-intensity exercise each week. There are currently no separate exercise guidelines for people who have gestational diabetes. But if you’re pregnant, start out slowly and gradually increase your activity level over time to avoid overdoing it.
Diabetes-friendly exercises include:
walking
swimming
dancing
cycling
Talk with your doctor about safe ways to incorporate activity into your diabetes management plan. You may need to follow special precautions, like checking your blood sugar before and after working out and making sure to stay hydrated.
Consider working with a personal trainer or exercise physiologist who has experience working with people who have diabetes. They can help you develop a personalized workout plan tailored to your needs

Homeopathic remedies derive from minerals, plants, or animals and people may consider them “all-natural.”
Homeopathic principles state that when someone dilutes a substance, that substance increases its therapeutic strength. The natural substance dilutes to the point where the remedy contains only trace amounts of the substance. People can then formulate it as:
•sugar pellets
•ointments
•drops
•creams
•tablets
There are examples of homeopathic remedies that people market to treat the symptoms of diabetes or prevent complications. These include:
Syzygium jambolanum or S. cumini (black plum) could help treat thirst, weakness, skin ulcers, and excessive urination.
Uranium nitricum might treat excessive urination, nausea, swelling, and burning with urination.
Conium (hemlock) may help treat numbness in the feet and hands, as well as diabetic neuropathy, or nerve damage.
Plumbum (lead) could help with numbness in the hands and feet, nerve pain, and tinnitus.
Calendula (marigold) might help treat infected ulcers.
Phosphoric acid may treat memory impairment, confusion or heavy head, frequent urination at night, hair loss, and difficulty maintaining an erection.
Candida (yeast) could help treat yeast infections.

Leave a comment