
What Is Glaucoma?
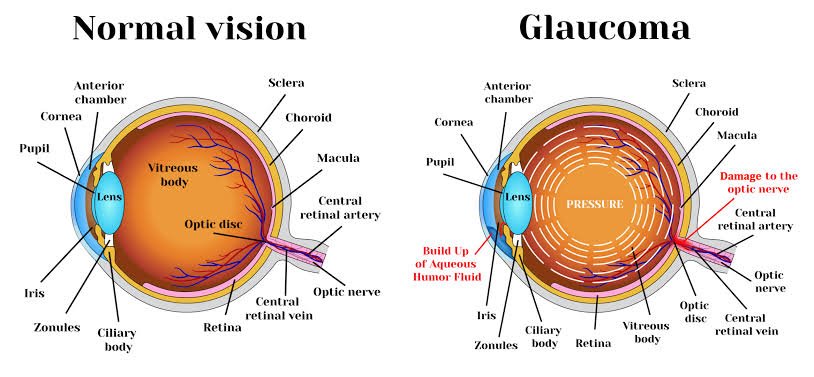
It’s a condition that can damage your optic nerve, usually because of the pressure in your eye. The optic nerve does an important job. It sends signals from your eye to your brain, which turns them into an image you can see. When the optic nerve isn’t working right, you’ll get problems with your vision. You can even lose your sight. The increased pressure in your eye, called intraocular pressure, can damage your optic nerve, which sends images to your brain. If the damage worsens, glaucoma can cause permanent vision loss or even total blindness within a few years.
Most people with glaucoma have no early symptoms or pain. Visit your eye doctor regularly so they can diagnose and treat glaucoma before you have long-term vision loss.
If you lose vision, it can’t be brought back. But lowering eye pressure can help you keep the sight you have. Most people with glaucoma who follow their treatment plan and have regular eye exams are able to keep their vision.
Glaucoma Causes
The fluid inside your eye, called aqueous humor, usually flows out of your eye through a mesh-like channel. If this channel gets blocked, or the eye is producing too much fluid, the liquid builds up. Sometimes, experts don’t know what causes this blockage. But it can be inherited, meaning it’s passed from parents to children.
Less-common causes of glaucoma include a blunt or chemical injury to your eye, severe eye infection, blocked blood vessels inside your eye, and inflammatory conditions. It’s rare, but eye surgery to correct another condition can sometimes bring it on. It usually affects both eyes, but it may be worse in one than the other.
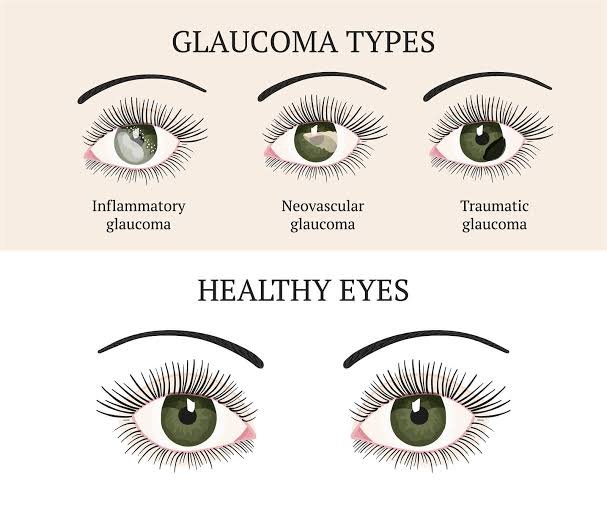


Types of Glaucoma
There are two main kinds:
Open-angle glaucoma. This is the most common type. Your doctor may also call it wide-angle glaucoma. The drain structure in your eye (called the trabecular meshwork) looks fine, but fluid doesn’t flow out like it should.
Angle-closure glaucoma. This is more common in Asia. You may also hear it called acute or chronic angle-closure or narrow-angle glaucoma. Your eye doesn’t drain like it should because the drain space between your iris and cornea becomes too narrow. This can cause a sudden buildup of pressure in your eye. It’s also linked to farsightedness and cataracts, a clouding of the lens inside your eye.
Less common types of glaucoma include:
Secondary glaucoma. This is when another condition, like cataracts or diabetes, causes added pressure in your eye.
Normal-tension glaucoma. This is when you have blind spots in your vision or your optic nerve is damaged even though your eye pressure is within the average range. Some experts say it’s a form of open-angle glaucoma.
Pigmentary glaucoma. With this form, tiny bits of pigment from your iris, the colored part of your eye, get into the fluid inside your eye and clog the drainage canals.

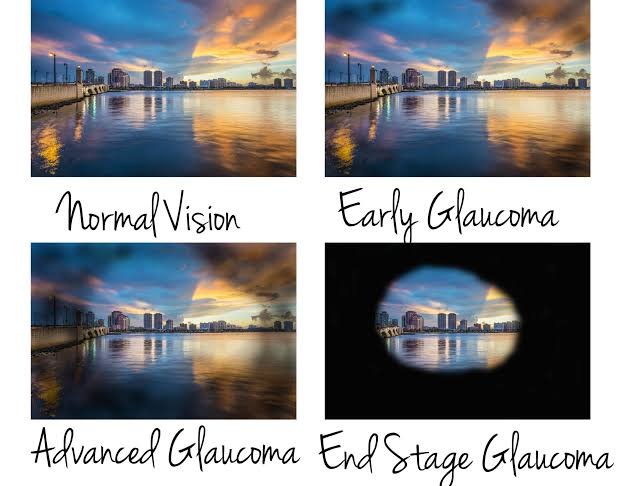
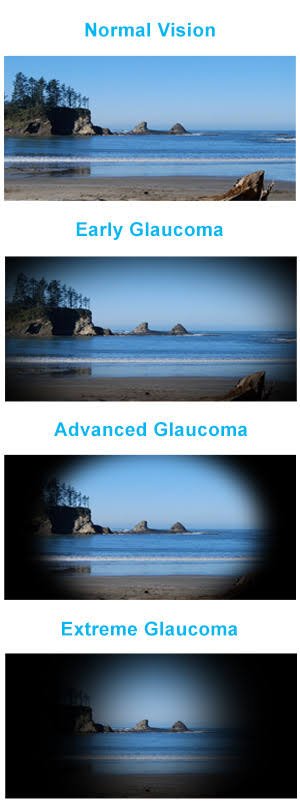
Glaucoma Symptoms
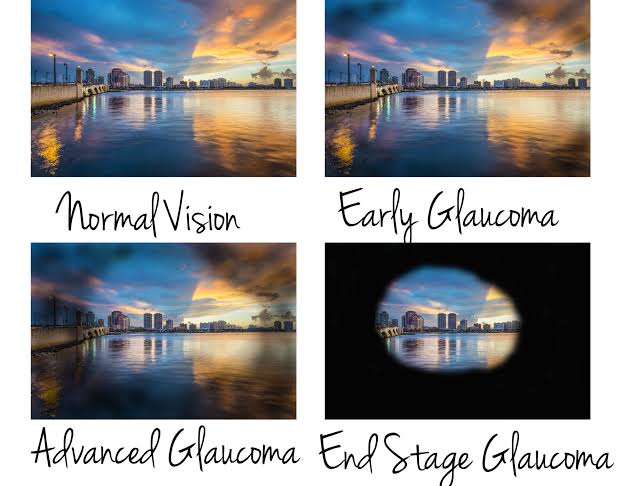
Most people with open-angle glaucoma don’t have symptoms. If symptoms do develop, it’s usually late in the disease. That’s why glaucoma is often called the “sneak thief of vision.” The main sign is usually a loss of side, or peripheral, vision.
Symptoms of angle-closure glaucoma usually come on faster and are more obvious. Damage can happen quickly. If you have any of these symptoms, get medical care right away:
•Seeing halos around lights
•Vision loss
•Redness in your eye
•Eye that looks hazy (particularly in infants)
•Upset stomach or vomiting
•Eye pain
Glaucoma Risk Factors
It mostly affects adults over 40, but young adults, children, and even infants can have it. African American people tend to get it more often, when they’re younger, and with more vision loss.
You’re more likely to get it if you:
Are of African American, Irish, Russian, Japanese, Hispanic, Inuit, or Scandinavian descent
•Are over 40
•Have a family history of glaucoma
•Are nearsighted or farsighted
•Have poor vision
•Have diabetes
•Take certain steroid medications such as prednisone
•Take certain drugs for bladder control or seizures, or some over-the-counter cold remedies
•Have had an injury to your eye or eyes
•Have corneas that are thinner than usual
•Have high blood pressure, heart disease, diabetes, or sickle cell anemia
Have high eye pressure
Tips for Living With Glaucoma
Glaucoma is a lifelong condition and needs continual follow-up with your eye doctor. There are other things you can do to help keep your eyes healthy.
Get moving. Regular exercise may help lower eye pressure and keep blood flowing to the nerves in your eye. Some activities can raise pressure, so talk to your doctor about the best exercise program for you.
Eat healthy. Enjoy a healthy, well-rounded diet. It won’t keep your glaucoma from getting worse, but it’s key to keeping your body and eyes healthy. Some studies suggest that food high in antioxidants can help when you have glaucoma. Eat more nutrient-rich foods like:
Dark, leafy greens
Fish that’s packed with omega-3 fatty acids
Take your medicine. Be sure to take your drops or pills exactly as directed. Set a reminder on your phone or watch so you don’t forget. Missing your meds could make your glaucoma worse.
Careful with contacts. You should be able to continue wearing contact lenses if you use medicated eye drops. But you may need to use some drugs when you don’t have lenses in. Also, some older medications can change your vision prescription. And if you need surgery, it may affect your ability to wear contacts.
Don’t smoke. It’s important to keep your body healthy, and nicotine takes a toll. Smoking also raises blood pressure and eye inflammation. That can make your risk of diabetes and cataracts go up. Both are risk factors for glaucoma. If you smoke, ask your doctor for advice on how to quit.
Watch your caffeine. Watch how much soda, coffee, and tea you drink. Too much caffeine can raise your eye pressure. One study found that just a cup of coffee could make the pressure in your eye go up a significant amount for up to 90 minutes.
Elevate your head. Use a wedge pillow when you sleep. It’ll keep your head raised just a little. That should help lower your eye pressure.
Drink fluids slowly. Don’t cut back on how much you drink, but spread out your beverages through the day. If you drink a lot at once, it can strain your eyes. Don’t have more than a quart at one time. Instead, sip small amounts.
Protect your eyes. Put on protective glasses when you work in the yard or play contact sports. Wear goggles when you swim. When choosing makeup, use non-allergenic brands, and replace items often. Be sure to wear sunglasses outside, especially in summer or around high-glare surfaces like sand, snow, and water. When you have glaucoma, your eyes can be very sensitive to glare.
Don’t rub. Glaucoma and the medicine you take might make your eyes feel itchy. But fight the urge. You can scratch them and make things worse. Ask your doctor if you can use drops to treat dryness.
Drive safely. Most people with glaucoma can still drive as long as they pass their state’s vision test. Simply put, your ability to drive will depend on how much vision has been lost. Some people with advanced glaucoma can get their license renewed with restrictions. Ask your doctor about whether driving will be a concern for you.
Be carefulwith yoga. You may need to reconsider some yoga positions. Some head-down moves that put your heart above your eye can raise your eye pressure. Research hasn’t shown that it makes glaucoma worse, but it’s not a good idea to do yoga positions that increase eye pressure. You may want to avoid poses such as:
Downward-facing dog
Standing forward bend
Plow
Legs up the wall
Glaucoma Prevention
You can’t prevent glaucoma. But if you find it early, you can lower your risk of eye damage. These steps may help protect your vision:
Have regular eye exams. The sooner your doctor spots the signs of glaucoma, the sooner you can start treatment. All adults need to be checked for glaucoma every 3 to 5 years. If you’re over age 40 and have a family history of the disease, get a complete eye exam from an eye doctor every 1 to 2 years. If you have health problems like diabetes or are at risk of other eye diseases, you may need to go more often.
Learn your family history. Ask your relatives whether any of them have been diagnosed with glaucoma.
Follow your doctor’s instructions. If they find that you have high eye pressure, they might give you drops to prevent glaucoma.
Exercise. Do moderate activity like walking or jogging at least three times a week.
Protect your eyes. Use protective eyewear when playing sports or working on home improvement projects.

HOMOEOPATHY MEDICINES
Homoeopathy today is a growing system and is being practiced all over the world. Its strength lies in its evident effectiveness as it takes a holistic approach towards the sick individual through promotion of inner balance at mental, emotional, spiritual and physical levels. When Glaucoma is concerned there are many effective medicines are available in Homoeopathy, but the selection depends upon the individuality of the patient, considering the mental and physical symptoms.
BELLADONNA
Glaucoma. Throbbing deep in eyes on lying down. Pupils dilated. Eyes feel swollen and protruding, staring, brilliant. Conjunctiva red; dry, burn. Photophobia. Shooting in eyes. Exophthalmus. Ocular illusions; fiery appearance. Diplopia, squinting, spasms of eyelids. Sensation as if eyes were half closed. Eyelids swollen. Fundus congested.
CEDRON
Shooting over left eye. Severe pain in eyeball, with radiating pains around eye, shooting into nose. Scalding lachrymation. Supra-orbital neuralgia periodic. Iritis, choroiditis.
COMOCLADIA GLAUCOMA
Glaucoma, sense of fullness. Eyeballs feels too large. Motion of eyes aggravates symptoms. Ciliary neuralgia with eyes feeling large and protruded, especially right. Worse near stove. Feels as if pressed outward. Sees only glimmer of light with left eye.
GELSEMIUM SEMPERVIRENS
Blurring and discomfort in eye. Dim sighted, pupils dilated and insensible to light. Orbital neuralgia with contraction and twitching of muscles. Bruised pain back of the orbits. Serous inflammations. Deep inflammations with haziness of vitreous. Eyes, red, sore aching, and suffused. Pain in eyes with or without lachrymation.
OSMIUM METALLICUM
Glaucoma, with iridescent vision. Violent supra and infra-orbital neuralgia. Violent pains and lachrymation. Green colors surround candle-light. Increase intra-ocular tension, dim sight, photophobia. Conjunctivitis.
PHOSPHORUS
Glaucoma. Thrombosis of retinal vessels and degenerative changes in retinal cells. Degenerative changes where soreness and curved lines are seen in old people. Retinal trouble with lights and hallucination of vision. Black points seem to float before the eyes. Patient sees better by shading eyes with hand. Fatigue of eyes and head even without much use of eyes. Green halo about the candle light. Atrophy of optic nerve.
PHYSOSTIGMA
Glaucoma; paresis of accommodation. Profuse lachrymation. Spasm of ciliary muscle, with irritability after using eyes. Vision dim, from blur or film; objects mixed. Pain after using eyes; floating black spots, flashes of light, twitching of eyelids and muscles of eyes. Nystagmus. Conjunctivitis.
PRUNUS SPINOSA
Glaucoma. Bursting pain in right eyeball shooting like lightning through the brain to occiput. Sudden pain left eye as if it would burst, better by lachrymation. Opacity of vitreous humor. Eyes feel as if bursting.
SPIGELIA
Eyes feel too large, pressive pain on turning them. Pupils dilated. Photophobia. Severe pain in and around eyes, extending deep into the socket. Ciliary neuralgia, a true neuritis.
Leave a comment